An Official White Paper From Gray’s Trauma Informed Care Services Corp WP NO. 200

Doctors of Behavioral Health (DBH) are considered healthcare innovators. They are healthcare disruptors. They are healthcare agents of improvement. That is to say, the role of the Doctor of Behavioral Health varies between different organizations. Many DBHs choose to work at major hospitals.
For example, they may work in heart health, obesity, smoking cessation, pediatrics, and primary care assistance. Nevertheless, while these arenas are great undertakings, there are still many paths that DBHs have yet to consider. For example, during my doctoral scholarship, there were many DBHs that had an interest in pursuing the mental health profession, as licensed psychologists.
While there was nothing wrong with these pursuits, when I took on a more mentorship role within my university, I encouraged students to pursue which ever endeavor suited their needs. Thus, if becoming a therapist was important to them, I explained the Clinical Psychology program was probably better suited for their needs. Then there were those individuals like me, who had come from a mixed population background. I encouraged students like this to consider becoming a Doctor of Behavioral Health. The versatility of the degree, allowed them room to move about the parts of the mental health profession that didn’t require licensure.
Versatility of Profession, Requires an Equally Versatile Degree
Practitioners, like myself, worked in fields like victim advocacy, patient advocacy, behavior analysis, the emergency department, and crisis intervention. Comparatively, many of us were from the world of crisis or violence prevention, and intervention. We had spent a lifetime working with medical, law enforcement, and mental health professionals. We worked a lifetime as integrated care professionals.
Most of us had reached the top of our careers. Moreover, we were either organization CEOs, executive directors, directors, or administrative management. As a result, we knew how to navigate our organizations. The wording within the DBH program description described a natural leap forward. While, many of us had already plateaued in our respective fields, the DBH degree offered us a new path forward.
Taking the Leap
The DBH degree gave many of us the versatility that we needed in our fields. The degree’s design allowed for more movement in the integrated healthcare community. One could accentuate their business acumen, while at the same time building an educational repertoire and background suitable enough for the medical community.
Doctors of Behavioral Health are Integrated Medical Professionals Who Can Fill the Vacancy
Moving up in the world of non-sworn law enforcement almost inevitably leads practitioners into four camps. Practitioners become executive directors, administrators, legal aid, or law enforcement. These are not bad professions. On the contrary, achieving these positions in the field of advocacy is nothing short of amazing. However, these camps can be expanded on. The DBH degree gives those in victim advocacy a way to fill professional vacancies, that otherwise are not occupied by individuals outside of the profession.
For example, when a victim is taken to the hospital, there is a possibility they will be assigned a victim advocate. What if the patient is a complex case. One can not just assign a licensed therapist to the individual. The individual may be injured badly and unable to do therapeutic intervention. Similarly, the patient may have a multitude of issues that are better treated by a Doctor of Behavioral Health, with various population certifications.
Making a Case for Doctors of Behavioral Health to Engage in Victim and Patient Advocacy in Medical and Mental Health Facilities
Victims of violence, especially intimate partner violence, are known to overutilize emergency departments (Gray, 2020; Keeling & Mason, 2008; Kleiner, 2006). These populations are complex, with co- and mutli-morbid conditions that physicians, untrained in how to care for victims of violence, find difficult to assess and treat (Gray, 2020; Keeling & Mason, 2008; Young-Wolff, Kotz & McKaw, 2016). Even though, primary care and emergency department physicians are trained and educated on how to treat the patient’s injuries; violence populations are still complex (Gray, 2020; Keeling & Mason, 2008; Wolff et al., 2016).
Yet, the totality of treatment is not appropriately taken care of in the medical or mental health settings (Wolff et al., 2016). A study at a Women’s hospital in Melbourne, discovered that 30% of 88 patients seen, were victims of domestic violence (Watson, Kenwood & Paauwe, 2015). As a result, at many medical facilities, primary care physicians have been looking for a solution to remedy the ongoing problem of domestic violence victims receiving inefficient care (Gray; 2020; Watson et al., 2015; Young-Wolff et al., 2016).
Doctors of Behavioral Health
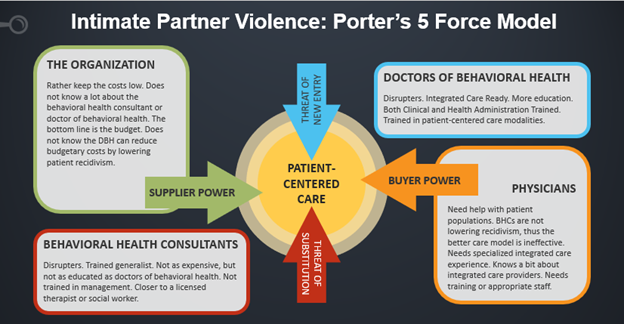
The 5-Force Model
The 5-force model above presents the four competitive forces that shape the patient-centered care that victims of domestic violence need (Gray, 2020). When it comes to medical facilities, physicians are sometimes knowledgeable about integrated care and its tenents. However, doctors of behavioral health and behavioral health consultants are still not fully known to medical institutions (Gray, 2020; Hunter, Goodie, Oordt, & Dobmeyer, 2017; Watson et al., 2015; Young-Wolff et al., 2016). Medical facilities want to keep costs low for the patient and themselves (Ogrinc, Headrick, Moore, Barton, Dolansky, Magdigosky, & Miltner, 2018). Doctors of behavioral health are trained in reducing utilization and fiscal management or other specialized skills (Gray, 2020; Cummings Institute, 2020).
Doctors of Behavioral Health Are Healthcare Disruptors: Generalists, Specialists, Trauma-Informed Providers, Educators, and Licensed Practitioners
Obesity, trauma-informed care, domestic violence in primary care, diabetes, culturally competent care, geriatrics, pediatrics, and women’s health are some of the specializations that doctors of behavioral health undertake (Gray, 2020; Cummings Institute, 2020; Arizona State University, 2020). Because of this, the doctor of behavioral health and behavioral health consultant are healthcare industry disrupters (Gaughran, 2020; Gray, 2020; Hunter et al., 2017). They have made a name for themselves, where there was originally none (Gaughran, 2020; Gray, 2020; Hunter et al., 2017).
The behavioral health consultant is a generalist, typically a licensed therapist (Hunter et al., 2017). They can be trained to take care of a multitude therapeutic needs a patient may have (Hunter et al., 2017). Albeit, the behavioral health consultant will refer approximately 20% of patients in primary care, to specialist trained to care for a specific population (Gray, 2020; Hunter et al., 2017). Unless a practitioner has specialization, credentialing or certification needed to care for a specific population, the practitioner may not be able to render services effectively (Gray, 2020).
Co- and Multi-morbid Issues Require Some Care from Specialization
In addition to this, intimate partner violence patients, who have extensive multi-morbid physical and mental health issues, need specialty care (Gray, 2020; Keeling & Mason, 2008; McNutt, Carlson, Rose & Robinson, 2002; Weiner & Moran, 1997). More integrated care providers, as well as specialist trained in caring for victims of violence, and trauma-informed care are needed in medical and mental health facilities (Forum on Global Violence Prevention, 2011; Gray, 2020; McNutt et al., 2002; Ko Ling & Cho, 2010; World Health Organization (WHO), 2020; Young-Wolff et al., 2016).
Is the Doctor of Behavioral Health What Victim and Patient Advocacy Has Been Waiting For?
Doctors of behavioral health have more education, specialization, training in quality measurement and improvement and population health management, than the behavioral health consultant (Cummings Institute, 2020; Gaughran, 2020; Gray, 2020). Because of their unique training in population health management, cultural competency, and care delivery, Doctors of Behavioral Health are the robust innovation that is needed within the medical and mental health industries, to provide efficient care for victims of violent crime (Arizona State University (ASU), 2020; Cummings Institute, 2020; Gray, 2020). In figure 2, below, it is clear to see why the doctor of behavioral health is best suited to treat intimate partner violence patients (Gray, 2020).
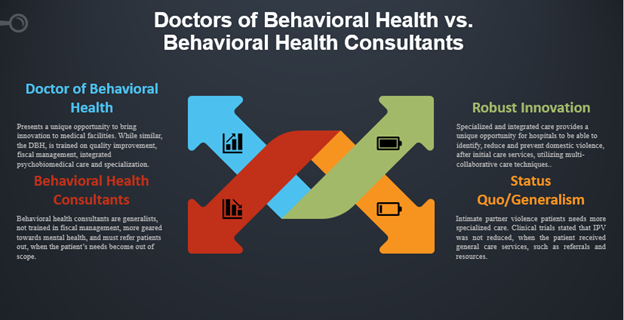
Doctors of Behavioral Health are Skilled and Effective Providers
Coupled with the extensive mental and physical needs of the IPV patients, doctors of behavioral health can assist hospitals in designing care delivery systems, best practices and improved performance measures that yield favorable outcomes (Cummings Institute, 2020). In addition to this, new, robust innovation is needed to tackle the vacancy left by generalism (Young-Wolff et al., 2016). Comparatively, the behavioral health consultant, doctors of behavioral health are trained in patient- and family-centered care and are versatile in the amount of mental health issues that can be treated (Hunter et al., 2017; Cummings Institute, 2020).
To clarify, with specialized training, doctors of behavioral health have more education and a higher level of skillsets to accommodate specialized population-based healthcare issues (ASU, 2020; Cummings Institute, 2020). Furthermore, Doctors of behavioral health are also trained in, disease management, cost savings and return on investment analysis, innovation in financing, entrepreneurship and intrapreneurship (Cummings Institute, 2020; Arizona State University, 2020).
The Bottom Line: Will Doctors of Behavioral Health Save Hospitals Money?
The bottom line is yes, Doctors of Behavioral Health save hospitals millions of dollars in the long run. Another key point is that the cost that intimate partner violence places upon healthcare facilities, justifies the hiring of a more trained, more skilled, more educated, and more specialized provider (Finlayson, Saltzman, Sheridan & Taylor, 1999; Gray, 2020; Watson et al., 2015; Weiner & Moran, 1997; WHO, 2020; Young-Wolff et al., 2016). As a result, The cost of treating IPV patients, including over-utilization of the emergency department and recurrent injuries, takes a financial toll on medical facilities (Finlayson et al., 1999; Gray, 2020; Weiner & Moran, 1997; WHO, 2020).
Below, figure 3 shows the medical costs of intimate partner violence within various countries. By comparison, the United States has a higher total cost, per capita, than other countries (Ko Ling & Cho, 2010). As a result, when one further reviews these findings, one is able to see that the collective medical cost of 4.9 billion is almost as great as the national average of the costs of IPV in the United States of 5 billion (Ko Ling & Cho, 2010; WHO, 2020). Also, one must note that the medical costs of IPV in Australia and New Zealand are much lower.
Figure 3: The Cost of Intimate Partner Violence
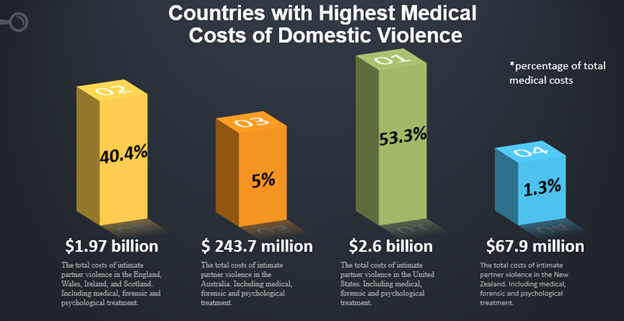
For example, Australia and New Zealand have collaborative care efforts in place to treat their IPV population (Gray, 2020; Ko Ling & Cho, 2010). In addition to this, they also utilize behavioral health care providers and community resources (Gray, 2020; Ko Ling & Cho, 2010). Consequently, even with these efforts, the medical costs of intimate partner violence is extremely high (Finlayson et al., 1999; Weiner & Moran, 1997; WHO, 2020). Therefore, using a specialized integrated healthcare provider, like a doctor of behavioral health, can reduce high medical costs, by allowing the provider to use their education, training and skills (Gray, 2020; Finlayson, Saltzman, Sheridan & Taylor, 1999; Watson et al., 2015; Weiner & Moran, 1997; WHO, 2020; Young-Wolff et al., 2016).
It Is Going to Take an Integrated Healthcare Team Effort
Even though one can only wish that healthcare was at a place in which it could say that we all work together as a team, we are not completely there yet. As a result, both the medical and the mental healthcare field have many positions which do not require licensure, the industries still create vacuums in which patients get insufficient care, due to lack of available providers. It takes a team to treat a victim of violence.
it is going to take an integrated healthcare team effort to treat victims of violence
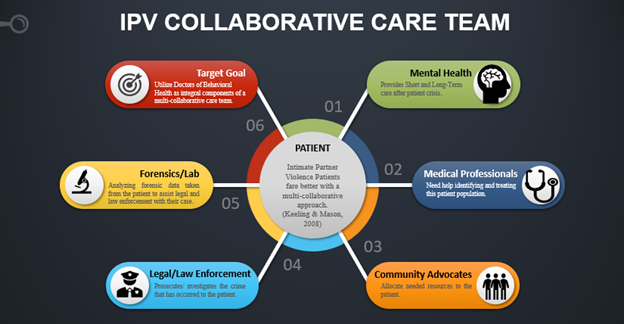
Victims of violence, like intimate partner violence patients, need medical and mental health providers to step up to the plate, to work together for the betterment of the patients (Gray, 2020). Whether it is a credentialed, certified or licensed professional, all team members do their parts to perfect the healthcare delivery process (Gray, 2020). Furthermore, Kleiner (2006) stated, that licensed individuals may have undertaken the proper educational steps to obtain licensure status, yet, this does not guarantee quality of service, nor retainment of knowledge.
A doctor of behavioral health not only has the management and administrative skillset, but also the clinical skillset to be able to tackle the extensive issues an IPV patients bring (ASU, 2020; Cummings Institute, 2020; Gray, 2020; Hunter et al., 2017). Because of this, the target goal for primary care facilities in the future should be to consider the doctor of behavioral health, as the right fit to assist primary care providers in taking care of the needs of patients who are victims of violence, and who are able to reduce costs for medical facilities (ASU, 2020; Hunter et al., 2017).
Sources:
Arizona State University (n.d.) Doctor of behavioral health degree. Arizona State University. Retrieved April 6th, 2020, from https://asuonline.asu.edu/online-degree-programs/graduate/doctor-behavioral-health-management/Cummings Graduate Institute. (n.d.) Doctor of behavioral health degree. Cummings Institute. Retrieved March 31, 2020, from https://cgi.edu/doctorate-of-behavioral-health/
Finlayson, T. J., Saltzman, L. E., Sheridan, D. J., & Taylor, W. K. (1999). Estimating hospital charges associated with intimate violence. Violence Against Women, 5(3), 313–335. https://doi.org/10.1177/10778019922181248
Forum on global violence prevention; Board on global health; institute of medicine; National research council. Social and economic costs of violence: Workshop summary. Washington (DC): National Academies Press (US); (2011). 6 Direct and Indirect Costs of Violence. Retrieved March 31, 2020 From: https://www.ncbi.nlm.nih.gov/books/NBK189992
Gaughran, K.R. (2019). 6 qualities all healthcare disruptors have in common. Healthcare Success. Retrieved March 31, 2020. https://healthcaresuccess.com/blog/healthcare-technology/healthcare-disruptors.html
Gray, A.D. (2020). Matrices for the utilization of doctors of behavioral health for patients who are victims of intimate partner violence. Retrieved April 3rd, 2020.
Hunter, C. L., Goodie, J. L., Oordt, M. S., & Dobmeyer, A. C. (2017). Integrated behavioralhealth in primary care: Step-by-step guidance for assessment and intervention (2nd edition). American Psychological Association.
Keeling, J., & Mason, T. (2008). Domestic violence: A multi-professional approach for health professionals. McGraw-Hill International (UK) Ltd.
Kleiner, M. M. (2006). Licensing occupations: Ensuring quality or restricting competition? W.E. Upjohn Institute for Employment Research.
Ko Ling Chan, & Cho, E. Y.-N. (2010). A review of cost measures for the economic impact of domestic violence. Trauma, Violence, & Abuse, 11(3), 129–143. https://doi.org/10.1177/1524838010374371
Mcnutt, L., Carlson, B., Rose, I., & Robinson, D. (2002). Partner violence intervention in the busy primary care environment. American Journal of Preventive Medicine, 22(2), 84-91.
Ogrinc, G. S., Headrick, L.A., Barton, A.J., Dolansky, M.A., Madigosky, W.S., Miltner, R.S. (2018). Fundamentals of health care improvement: A guide to improving your patient’s care (Third edition). Joint Commission Resources ; Institute for Healthcare Improvement.
Watson, A., Kenwood, A., Van Paauwe, P. (2015). Domestic violence training model for hospitals: a toolkit to help hospitals train staff to appropriately identify and respond to family violence will be available in coming months. Australian Nursing & Midwifery Journal, 23(2), 13. Retrieved from https://link-gale-com.ezproxy1.lib.asu.edu/apps/doc/A426902388/CWI?u=asuniv&sid=CWI&xid=ece10bfb
Weiner, D., Moran, P. (1997). Responding to domestic violence: A coordinated response by a consortium of teaching hospitals. Domestic Violence Task Force, Conference of Boston Teaching Hospitals. Academic Medicine, 72(1), S59-64.
WHO | The economic dimensions of interpersonal violence. (n.d.). WHO. Retrieved March 31, 2020, from https://www.who.int/violence_injury_prevention/publications/violence/economic_dimensions/en
Young-Wolff, K., Kotz, K., & Mccaw, B. (2016). Transforming the Health Care Response to Intimate Partner Violence: Addressing “Wicked Problems”. JAMA, 315(23), 2517-2518.
