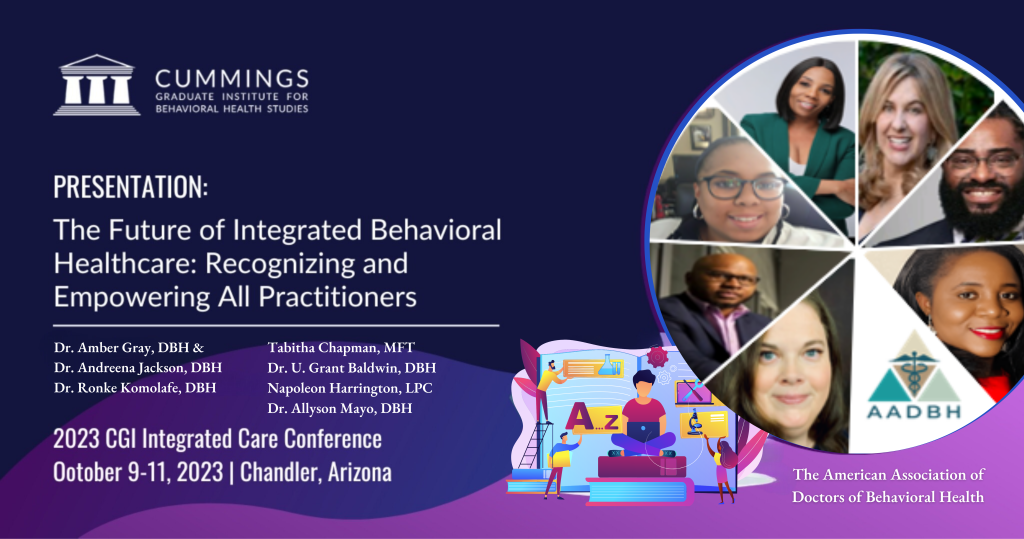
The American Association of Doctors of Behavioral Health Will be Presenting at the Cummings Graduate Institute’s Integrated Healthcare Conference
The AADBH is set to play role in furthering discussions on integrated health at the CGI conference. So, we are excited to share that we will be hosting a panel discussion. The panel features select board members who will delve deep into their individual and collective contributions to integrated health. Moreover, their insights promise to illuminate the path forward in holistic patient care and multidisciplinary collaboration. Additionally, the AADBH will have a dedicated table at the conference venue. This platform will serve as a touchpoint for attendees to interact with our representatives. Participants can seek clarifications and gain deeper insights into our initiatives. Further, we’ll be using this opportunity to encourage and facilitate new memberships. We invite students and professionals to join our mission in advancing behavioral health within the integrated care paradigm.
Register to Join the AADBH at the Conference
Register: https://cgi.edu/conference

The CGI Integrated Health Conference, scheduled for October 9-11, 2023, in Chandler, Arizona. This conference is a premier event tailored for a wide array of professionals in the healthcare domain. Its audience spans multidisciplinary integrated professionals. For example, leaders, and researchers to those involved in many aspects of healthcare design, delivery, and enhancement will be in attendence. The conference welcomes Doctors of Behavioral Health (DBHs) or students pursuing DBH. They also welcome related healthcare fields, faculty, subject matter experts, and researchers specializing in integrated care. In addition, the event is an invaluable experience for mental health professionals, social workers, community health workers, nursing experts, physicians, and specialists.
Tabitha M. Chapman Honored with Karen Cooper Lifetime Achievement Award for Beloved Community Advocate
Lake Elsinore, CA 06/01/2023 – The Partnership Awards held by the California Partnership to End Domestic Violence, is honoring Tabitha M. Chapman with the esteemed Karen Cooper Lifetime Achievement Award for Beloved Community Advocate. This distinguished honor is bestowed upon individuals who have made remarkable contributions to addressing domestic violence and championing the cause of victims within their communities. Chapman’s outstanding leadership, dedication, and substantial impact in the victim services and domestic violence field have rightfully earned her this esteemed recognition.
Chapman founded, “The Freedom Train Project Inc.,” a non-profit entity that helps victims of coercive control, and cultic abuse. Her profound influence stems from her unwavering commitment to providing comprehensive mental health and victim advocacy services to victims of cultic abuse. Through her tireless efforts, she has bridged the gap between domestic violence agencies and other victim services providers, ensuring that survivors receive the support they desperately need.
Her visionary collaborations have empowered victims within their respective communities, equipping them with vital resources and fostering healing in the face of trauma. By recognizing Chapman’s achievements, the Karen Cooper Lifetime Achievement Award celebrates her remarkable dedication and passion for improving the lives of those affected by cultic abuse, domestic violence, human and sex trafficking, post separation abuse, and institutional abuses.
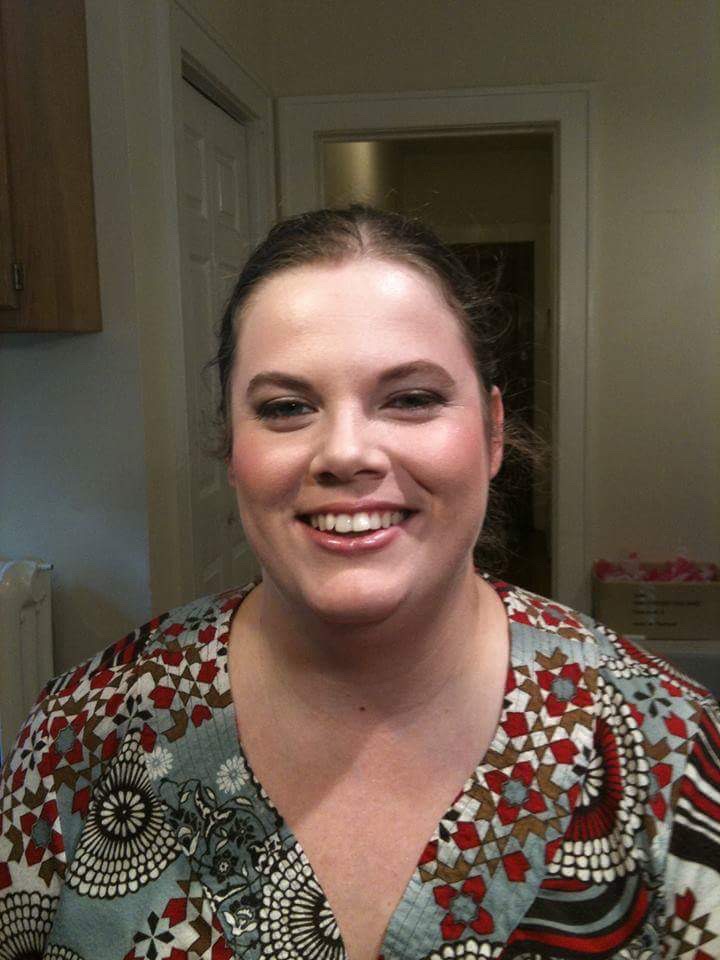
Throughout her illustrious career, Chapman has consistently displayed exemplary leadership, advocacy, and unwavering support for victims. Her profound impact on the victim services and the emerging cultic abuse advocacy field cannot be understated. Her approach has been centered on not only addressing immediate needs but also creating sustainable solutions for long-term healing.
Chapman’s unwavering commitment to getting victims the help services they need has made her a respected and influential figure in her field. Her efforts have transformed the lives of many survivors, providing them with a renewed sense of hope and the tools necessary to rebuild their lives after experiencing cultic abuse.
The Karen Cooper Lifetime Achievement Award for Beloved Community Advocate serves as a testament to Chapman’s outstanding efforts. By recognizing her exceptional achievements, the award acknowledges the transformative impact she has had on victims’ lives and the broader community.
Upon hearing of the nomination and honor for the award, Chapman expressed her deep gratitude and emphasized the importance of collaborative efforts in combatting domestic violence. She said, “I am truly humbled and honored to receive the Karen Cooper Lifetime Achievement Award. I can’t believe I received it.”
As Tabitha M. Chapman continues to champion the rights of victims and collaborate with organizations to address cultic abuse, her legacy will endure, inspiring future generations to strive for a society free from abuse and filled with compassion. Chapman will be honored at a ceremony with the California Partnership to End Domestic Violence, where she will receive the Karen Cooper Lifetime Achievement Award for Beloved Community Advocate.
Congratulations Tabitha M. Chapman!

FOR IMMEDIATE RELEASE
Riverside County resident honored with statewide award for domestic violence advocacy
work.
Dr. Amber Gray, President and Healthcare Educator of Gray’s Trauma-Informed Care Services Corp, awarded for work “fighting for justice for marginalized communities by working on changing the way providers and organizations service these communities.”

July 22, 2022 – SACRAMENTO: The California Partnership to End Domestic Violence (the Partnership), a coalition representing over 1,000 survivors, advocates, organizations, and allied individuals, honored Lake Elsinore resident Dr. Amber Gray with the Equity Award at a virtual ceremony. Dr. Gray is a community leader that empowers agencies like the Freedom Train Project Incorporated, serving survivors of domestic, sexual, and other forms of abuse by connecting them with donations, volunteers, and resources. This has been especially valuable during ongoing staffing and supply shortages brought on by the COVID-19 pandemic. Additionally, Dr. Gray provides trauma-informed education to primary care providers in order to prevent the further traumatization of survivors in the healthcare setting, among many other efforts to build positive relationships with underrepresented agencies and community members working toward ending domestic violence.

Violence, Statewide Equity Award, for the work that she does in Domestic Violence Advocacy
“Dr. Gray is always fighting for people who do not have a voice. She has been innovative in the ways in which she helps those who need to be heard. Though she is 1,010% dedicated to victims of domestic violence, Dr. Gray is always fighting for those who need help. She has been doing this work for nearly three decades. I don’t think she will ever stop.” said Rebecca Ax, a Western Region Sexual Assault Coordinator for the United States Marine Corp. In her
nomination of Dr. Gray, Rebecca also stated, “Helping build equity and working for the underrepresented is in Dr. Gray’s DNA. She will network with whoever she needs to, to make sure that the communities or individuals have what they need.”

Throughout her career, Dr. Gray has committed to a philosophy of empowering communities with education, resources, and charitable contributions in order to be competitors and future allies in the fight to end domestic violence, and violence against women globally. Aside from starting the Volunteer Services Unit at Gray’s Trauma-Informed Care Services Corp and ensuring that many agencies receive assistance with staffing and funding, Dr. Gray is also a collaborative author of the book, “Women and Violence: Global Lives in Focus.” Dr. Gray demonstrates a life-long commitment to learning and is pursuing a second Doctorate in Psychology, Public Policy, and Law to understand how public policy can “help shift the narratives to bring equitable change in systems that treated people with injustice.” Dr. Gray has also received numerous accolades, aside from this recent win, including congressional awards, letters of commendation from the senate, as well as awards and nominations from various organizations, for outstanding work and achievement in violence prevention and domestic violence.
In reference to her numerous community-building efforts she stated, “If you embolden people who have no one to speak to their good deeds, their hard work, and their good nature, and you provide them resources to remove that deficit, the individuals will go on to thrive and help others who may not be receiving equitable treatment as well.”
#
About the Partnership
The California Partnership to End Domestic Violence (the Partnership) is California’s recognized domestic violence coalition, representing over 1,000 survivors, advocates, organizations and allied individuals across the state. Working at the state and local levels for nearly 40 years, the Partnership has a long track record of successfully advocating for over 200 pieces of legislation on behalf of domestic violence victims and their children. The Partnership believes that by sharing expertise, advocates and legislators can help end domestic violence. Through our public policy, communications and capacity-building programs, we create system-wide change that supports survivors and invests in prevention. Every day we inspire, inform and connect all those concerned with this issue, because together we’re stronger. With offices in Sacramento, the Partnership’s member programs span the entire state. For more information,
visit www.cpedv.org
“If you embolden people who have no one to speak to their good deeds, their hard work, and their good nature, and you provide them resources to remove that deficit, the individuals will go on to thrive and help others who may not be receiving equitable treatment as well.”
said Dr. Gray, when asked about her community-building efforts.
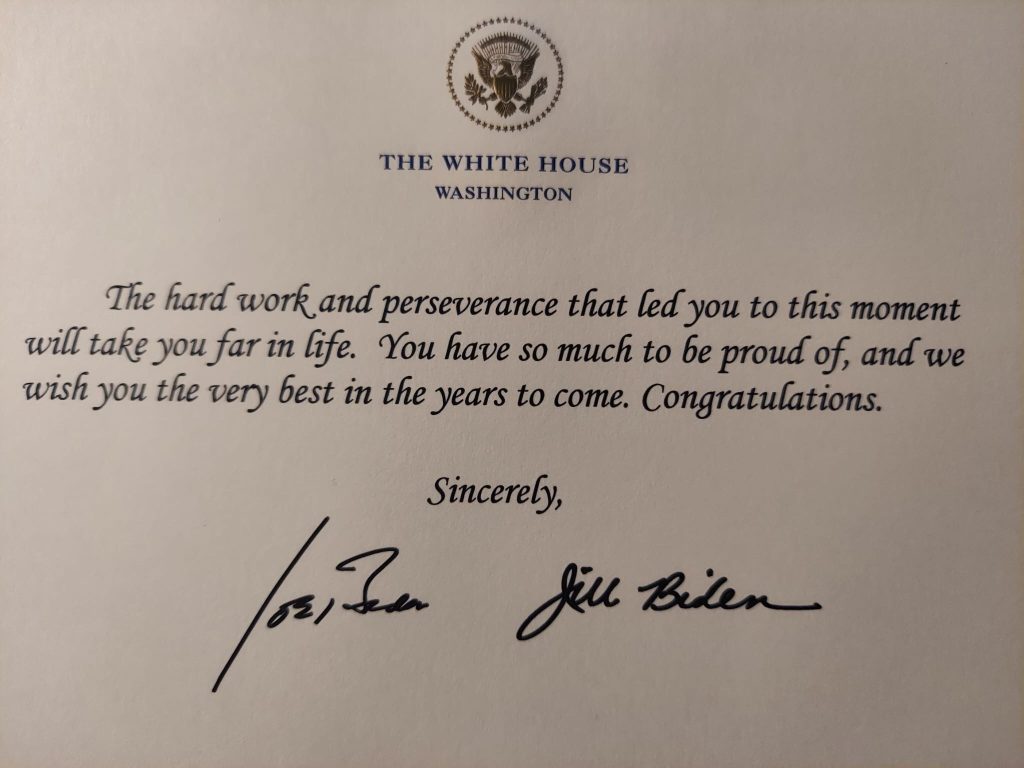
A Word From Gray’s Trauma Informed Care Services Corp Staff: In addition to the wonderful acknowledgment from the California Partnership to End Domestic Violence, Dr. Gray received a Presidential greeting for her hard work and earnest efforts. It is always a pleasure to work with Dr. Gray. She has many coals in the fire, and astonishingly gets a lot done in a short amount of time. Working as the CEO of this organization, Dr. Gray has tried to achieve the impossible, during a pandemic, post-pandemic, inflation, social unrest, societal violence, covid-surge, the rise of monkey pox, and personal family losses and illness.
Still, she has selflessly pushed forward, being a voice for those who do not have a voice. In her work with the Freedom Train Project Incorporated, Dr. Gray continues to work hard behind the scenes to be a voice for victims of cultic abuses. At the Freedom Train Project Incorporated, Dr. Gray works as the Director of Violence Prevention and Victim Advocacy (DVP-VA). In this capacity, Dr. Gray has worked with the Executive Director to create programs, and educational materials to help the organization create new and innovative ways to help victims heal after cultic abuse. We can’t say enough how proud we are of our beloved CEO. It is not always easy. We know. Yet, if anyone has taught us that doing the work that matters for victims of violence is hard, it is you. We know its difficult. Keep doing what you do Dr. Gray. You are making a difference. Congratulations, Dr. Gray!
A Message from the CEO and Staff Regarding the Recent Decision Overturning Roe v. Wade by the Supreme Court of the United States of America

June 24th, 2022
At Gray’s Trauma-Informed Care Services Corp, we are vehement opposition to the decision made by the Supreme Court to overturn Roe v. Wade. For victims of domestic violence and sexual assault, having bodily autonomy is imperative. There are rights that are fundamental to the physical and mental well-being of these populations. As an organization that is wholly dedicated to victims of rape, incest, victims of violence, those with trauma, and individuals being in full control of their healthcare decisions, Gray’s Trauma-Informed Care Services Corp is appalled by the decision to overturn Roe v. Wade.
For decades, there has been a legacy, from a small majority, that wishes to keep reproductive oppression woven throughout the legislative, executive, and judicial branches of this country. This keeps the law, courts, and country, more partisan and less objective. This is unacceptable. Overturning Roe v. Wade will not stop abortions, but it will make people seek out less safe abortions. We know this story. This is history repeating itself, which means we, as a society, have learned nothing. As people continue to seek out and obtain abortions, Gray’s Trauma-Informed care Services Corp will make sure that people know how to have access to safe abortion practitioners. We will continue to support those who need psychobiomedical care, despite the Supreme Court ruling.
The California Partnership to End Domestic Violence had some facts and reflections that they wanted people to keep in mind. We here at Gray’s Trauma-Informed Care Services Corp thought these facts and reflections were worth sharing:
- Abortion is currently protected by law in California. Keep any appointments you have.
- Survivors are already denied bodily autonomy in abusive relationships; this decision will block many survivors throughout the nation from accessing abortion and reproductive health services.
- This decision is an intentional attack on the liberties of LGBTQIA+, Black, Indigenous & Native, Latinx/Latine, and AAPPI women & gender-expansive people.
- This decision sets a dangerous legal precedent that violates the right to privacy.
- It is critical to hold space for women-identified and gender expansive people today, who are experiencing heartbreak, anger – especially activists who gave their energy to establishing these rights.
In the days, weeks, months, and years to come, we will all have to do our parts, to continue to help people to be free from trauma and re-traumatization. Keep fighting the good fight. Do not lose hope. We will keep fighting for reproductive justice and healthcare autonomy for all.
Gray’s Trauma-Informed Care Services Corp is proud to be a California-based corporate organization, where we provide healthcare education, leadership and personal development, advocacy, volunteer, and resource services for victims of violent crimes, including, domestic violence, medical abuse, child abuse, human trafficking, veterans, LGBTQIA+, and victims of sexual violence. We will continue to provide our services despite appalling and controlling decision made by SCOTUS. We will assist people who need safe integrated healthcare services, always.
Resources, Statements, and Calls to Action
https://www.sistersong.net/reproductive-justice
https://www.plannedparenthoodaction.org/
https://www.reproductivefreedomca.org/
Mental Health Services: A Message from NAMI….. As you process today’s news, know we are here for you. To anyone who needs support, our HelpLine is available at 1-800-950-NAMI (6264) – open Mon-Fri from 10 am to 10 pm ET or text “NAMI” to 741-741.
_______________________________________________________________________________________________
A Message from the CEO and Staff Regarding Recent Violence

It is with utmost consideration and regard to the recent inexcusable acts that took so many innocent lives at Robb Elementary School shooting, The Topps Grocery Store shooting, the Laguna Woods Church shooting, the Christchurch shooting, and the violent war crimes happening in the Ukraine, that Gray’s Trauma-Informed Care Services Corp (GTICSC) offers its sincerest condolences. Our hearts go out to everyone who has lost loved ones. Our staff, is deeply saddened by the violence the people of our country have endured.
Our country has experienced multiple hate crimes, only 10 days prior to the tragedy in Uvalde and there have been senseless violent acts, around the world. We have all witnessed, experienced or have been triggered by the pointless and irrational loss of human life. All of these tragedies occurring amidst a worldwide pandemic and epidemic outbreaks. Our citizens watch the news, and see nations engaged in war, again with children being some of the saddest and most innocent causalities. For now, we can only offer our sincerest regards to the family and friends who have lost their lives. We stand with the survivors left in the aftermath. We grieve in pain with the people who lost their family members at the hands of a white supremacist. We grieve in pain with the parents, educators, and individuals vested in improving the lives of others, who are struggling to understand the acts of violence around them. We are thankful to the first responders, law enforcement, and all those who tried to help stop this most recent tragedy. Through this month of May…mental health awareness month, we are also worried about those who are not doing well with all that is happening around the world.
Therefore, we urgently call those who are struggling with thoughts of harming themselves or violence toward others to seek assistance tonight. These difficult times call for recognizing the strength in seeking support. If you or someone you know is struggling, please request guidance from an appropriate professional. We here, at Gray’s Trauma-Informed Care Services Corp know how to get you the help you need. We are here to offer compassion and assistance to all who seek support. If you have any questions, please reach out to us at DrGray@gettraumainformed.com or info@gettraumainformed.com and we will do our best to assist. For those who may need someone to talk to, you may call the NAMI HelpLine
NAMI
https://www.nami.org/help at 800-950-6264 or chat https://www.nami.org/help
with them M-F, 10 a.m. – 10 p.m., ET. In a crisis, text “NAMI” to 741741 for 24/7, confidential, free crisis counseling.
DISASTER DISTRESS HELPLINE/SAMHSA
You can also call Disaster Distress Helpline/SAMHSA Phone: 800-985-5990 (for Spanish, press 2). Text “TalkWithUs,” to 66746.
NATIONAL CENTER FOR VICTIMS OF CRIME
You can also call the National Center for Victims of Crime
VictimConnect 855-4-VICTIM (855-484-2846) 8:30 am – 7:30pm ET
NOVA
www.trynova.org/help-for-crime-victims
NATIONAL MASS VIOLENCE VICTIMIZATION RESOURCE
See more Resources in Our Website’s Resource Section
Please check back for updates on additional resources and articles offering guidance from our Paragon e-Magazine authors.
Respectfully,
Dr. Amber D. Gray, DBH
CEO
&
The Gray’s Trauma-Informed Care Services Corp Staff
The Volunteer Services Unit Program

Gray’s Trauma-Informed Care Services Corp, became a Certifying Organization for the Presidential Volunteer Service Award (PVSA) last year, in 2021. We decided that one of the greatest gifts that we could give back to the community was to create a volunteer services program, in which individuals could work to help those in need. Individuals in the volunteer services unit are eligible for a limited edition minted Gray’s Trauma-Informed Care Services Corp challenge coin, as well as hours accumulated for the PVSA.
Our “Trauma-Informed World,” medallion is a 2″ coin, with a roped edge. It is made of black nickel and features our organizations name, logo, the earth and has a limited edition number on it. The coin is given to those who go above and beyond in their service to others. We are hoping that by creating opportunities to be recognized for merit, we can increase volunteer service to others. Our organization is continuing to partner with advocacy agencies, that we may be able to continue to help those in need. If you are interested in volunteering with our organization, please contact us at: volunteer@gettraumainformed.com
We Have Become a Pink Partner!

For the month of October, Gray’s Trauma-Informed Care Services Corp has been making big changes and doing a lot of things differently. One of those things is how we raise awareness, who we partner with and how we support great organizations. The mainstay of our business is advocating for victims of violent crime and bringing innovation and change to healthcare practice and policy through evidence-based education. Every October, our organization did an awareness Walk/Run for those who had been effected by breast cancer. However, given the complexities of the era that we are in, our organization felt that we needed to do more. We decided to become a pink partner for the Susan G. Komen foundation.
What does it mean to be a pink partner? Our organization plans to raise awareness about breast cancer and hold fundraisers to further the efforts of the Susan G. Komen foundation. By becoming a pink partner, Gray’s Trauma-Informed Care Services Corp has taken the first step towards a world without breast cancer by raising funds to stop this disease that affects 1 in 8 women during their lifetime. As the world’s largest and most impactful breast cancer organization, Susan G. Komen funds more breast cancer research than any other nonprofit, while providing real-time help to those facing the disease.

Our fundraiser is called the Diane Mack Pink Promise Event. It was created in honor of an extraordinary woman, whose life was cut short by an aggressive form of breast cancer. Diane Mack was a single mother, a loyal and dedicated worker of the county of Los Angeles, and she brought happiness and joy to anyone who had the pleasure to make her acquaintance. After her death, her family made a promise to fight breast cancer where ever and whenever they could.

Inspired by the family’s efforts, Gray’s Trauma-Informed Care Services Corp decided to host the Diane Mack Pink Promise Event, a Susan G. Komen fundraiser. You too can join the cause by donating to the event. This event will become a staple of Gray’s Trauma-Informed Care Services Corp’s annual awareness events.
To Participate, please click the link below:
http://www.info-komen.org/goto/DianeMackPinkEvent
Let’s all work to put an end to breast cancer once and for all.
Q&A With Dr. Gray Part One: On Victim Advocacy and Services

By Noble Baycar Editor Tabitha M. Chapman, CVA
Dr. Gray was asked to answer questions victim advocacy and service providers had about working within the industry. While she was asked several questions, the most interesting questions were chosen to be featured here in the Newsroom. We hope that you learn a lot from the information presented. If there are questions regarding victim advocacy, victim services, violence prevention and intervention and victim assistance, please email DrGray@gettraumainformed.com and you may see your question featured in a Newsroom Q&A with Dr. Gray session.
What is the number one issue an agency should be concerned with?
I think the number one issue that any agency should be concerned with is safety. No matter what an agency does to ensure the safety of the individuals the entity caters to, or for the individuals the organization is servicing, one can never be too safe. Safety is a huge broad topic with different layers of issues that providers must think about. For example, an organization might have their physical layout secure, but might be missing risk factors within the facility, such as non-secure phone lines, problematic technology that may expose a client’s identity or any other type of risk factor that is being overlooked. Safety is not just about having an armed guard outside to protect those who are within a facility. Safety is also about minimizing risk before they happen or eliminating the risk all together. Safety and its many facets, is the number one issue an agency should be concerned with.
Do you feel as though there should be an overseeing body, like the BBS, within victim services?
The short answer is no. There shouldn’t be an overseeing body within victim services due to the fact that victim services is population health management and public health driven. Different locales, areas and regions, or even different national organizations have varying issues of concern that they focus on. With limited funding, tightly budgeted allocation of monies, and not enough grants issued out, various victim services entities have to do what is best for them, to meet the needs of their population. Different areas also need different amounts of money to provide human, victim and social services, so that they continue to meet government requirements. With all of the variation of needs, an overseeing body, would simply make the landscape to compounded with issues. An overseeing body that is using a one size fits all model, is not going to effectively and efficiently, parse out service to victims and much needed resources to the providers, who rely on those resources. Victims will not get the best quality of service as they would if independent bodies place money and resources where they will work best for the population. This is not to say, that victim services does not require oversight. On the contrary, there are many credentialing, education, training, and certification agencies, dedicated to making sure that individuals are highly qualified to do their jobs. Having a governing licensing body, does not bring professionalism to the industry. Having an effective and efficient system that works for its population and providers does. So, I believe our focus should be on maintaining that quality and continuously improving upon the issues that we are able to.
What’s the best way to deescalate the situation?
This is a tough question. It depends on the situation. I know that’s a cliche answer. However, the best way to deescalate the situation is somewhat based on what’s happening within that situation. In tumultuous situations, a victim services provider is going to have to utilize the skills that they learned in their trainings to deescalate a situation that may arise between themselves and a client, between clients, or provider to provider. In general, deescalating a situation requires thinking that situation through, looking at the best options that are presented, not acting, before thinking; being mindful of ones own thought processes and thinking about not only the needs of the client, but adhering to the standards, ethics, vision and mission of one’s organization. If a situation is going to put you into a position where your actions are going to escalate the situation or go against the principles of your organization, you may want to make different choices and be cognizant of ethical standards, while making your decision. Again, one can’t really say what the best way to deescalate a situation is, unless they know what the parameters of the situation is.
What can be done about backbiting in small organizations?
In a nutshell, the standards and practices of an organization, will produce the environment in which providers have to work. If there is backbiting within the organization, something about the agency is problematic. Different people have different personalities, and different personalities behave differently in given situations. This being said, an organization can implement policies, rules and regulations, higher standards and better channels of communication to help combat the problem. Backbiting usually results out of jealousy, anger and communication breakdowns. If you want to end backbiting it’s best to go to your administrators and present issues that you may be having, allow your administrators to have a chance to work through those issues to help your organization maintain a more cohesive staff and a better understanding of what issues everyone is dealing with. Stress, in and of itself, can be a catalyst for communication breakdowns. Being forthcoming and hashing out issues, is beneficial to all parties involved.
Why isn’t the field broader?
I would actually argue that the field is quite broad. Our industry spans through most human and social services arenas. This includes, but is not limited to law enforcement, legal, human, victim, social, and child services, healthcare and therapeutic services. I think that maybe the question is why is it that advocacy, as a profession, is not more known? People don’t know victim advocacy and victim services can be a lifelong career. When people go into psychology, they are only taught about therapeutic mental health, and every industry around that, is treated as though it is nonexistent, when those other industries are the bulk of behavioral and mental health services. Twenty-six years ago, I myself, didn’t even know victim advocacy was a career. I can’t think of working within any other industry. Even when I first started, Victim Advocacy and Services had credentialing and certifying bodies that ensured that individuals had the right skills and education to perform their duties. Today our industry gets conflated with the therapeutic side of mental and behavioral health services. I believe that as organizations, such as, Gray’s Trauma-Informed Care Services, works to improve upon industry standards, practices and empowering providers, more victim advocacy and services agencies will be able to sort these issues out for newcomers to the profession.
What can we do to make victim advocacy and victim services professions more known in the future?
Bringing awareness to the fact that, outside of therapeutic healing and therapeutic mental health services, there is an entire world of mental and behavioral health services, that individuals encounter before they ever step foot into a therapy services office. By encouraging academic institutions and the schools of psychology, anthropology, criminal justice, and other human and help services arenas, to bring awareness to the world outside of therapy, I believe this would be the change more victim services agencies would benefit from. The victim advocacy and services industry already is standardized, ethical and has codes of conduct. What is needed are more advocates, who want to do the work of professional advocacy, and not just as a springboard into therapeutic services.
How do I deal with someone when they are crying, and I am not a therapist?
The best way to do this is to realize that you have more tools in your toolbox than you are giving yourself credit for. Let me break this down. The job of a therapeutic service provider is to provide therapeutic services. The job of a victim advocate or victim assistance provider is to guide and help a victim through the legal, social and law enforcement process that is happening to them. As a Victim Services Provider (VSP), your job is to ease the victim’s worries and fears. You are to help them to understand the process that they are in. If an individual is crying, that is normal. The process is difficult. They could be losing their home, their children, their job, or any number of events that happens on this journey to safety. As a provider, you can utilize the motivational interviewing strategies you learned in basic, intermediate, advanced or specialty advocacy training. You can empathize with the victim, explaining you know that it is a daunting process, but it is also short-term. You can take them step by step, on what will happen next. This will quell some fears and give the victim a bit of a break from the worries of the unknown. You can tell your client how the process is going to work and assure them, that if they have any questions, you are there to help. If you are worried about their mental health status, you can let the client know, that there are licensed professionals who can help them with their distress, anxiety, and mental health. There is nothing wrong with letting your client know they can receive care beyond the scope of what I could provide. This is what the therapeutic community is there for. Remind your client that you are there to get them safely through this process. You are a victim assistance provider; it is your duty to alleviate the clients worries. It is not so much that you’re not a therapist, it is more that you have to use a different set of skills than a therapist would to effectively and efficiently help your client in a limited amount of time.
This concludes part one. Keep an eye out for Part Two of Q&A with Dr. Gray on Victim Advocacy and Services. Remember, if you have questions regarding trauma-informed victim advocacy, services, assistance and violence prevention, to email DrGray@gettraumainformed.com
TRAUMA-INFORMING INSTITUTIONS TO COMBAT OLD AND OUTDATED PRACTICES
By Dr. Amber D. Gray
July 2020
Recently, there has been much discussion over what trauma-informing facilities will do for individuals. From CEOs to operational staff, people are looking for ways to combat practices that are outdated and not beneficial to society. Since trauma informing providers began, research has shown an increase in the benefit that the new ideology, methods and techniques provide. Institutions all over the U.S. involved in human, behavioral or mental health services, have been clamoring to get their staff trauma informed (Kelly-Voicu, 2020). Being trauma informed is not going to go away any time soon. While the buzz usage of the phrase, “trauma informed,” will phase out in time, the ideologies, methods and techniques will not. Here is why: According to Dr. Monique Tello, of Havard Health Publishing, “trauma informed care is practicing a culture of safety, empowerment and healing.” Being able to reach a patient where they are at, to meet their needs, is not only beneficial for healthcare practitioners, but for all those who work with or interact with people. There will be those who toss the phrase around, ad nauseum. Yet, those who are in the business of helping people to heal, caring for patients, and improving health, will continue to use trauma informed practices to make care more effective and efficient.
Source(s):
Doctors call for trauma-informed healthcare in fight against systemic racism. (2020, June 15). Queens County Politics. https://www.queenscountypolitics.com/2020/06/15/doctors-call-for-trauma-informed-healthcare-in-fight-against-systemic-racism/
MPH, M. T., MD. (2018, October 16). Trauma-informed care: What it is, and why it’s important. Harvard Health Blog. https://www.health.harvard.edu/blog/trauma-informed-care-what-it-is-and-why-its-important-2018101613562
THE BRANDON ACT PASSES, MAKING IT EASIER FOR SERVICE MEMBERS TO SEEK HELP OUTSIDE OF THEIR CHAIN OF COMMAND
By Dr. Amber D. Gray
June 2020
The passing of the Brandon Act will make it easier for service members to receive mental health assistance outside of their chain of command. In 2018, Navy Aircrew Aviation Electrician’s Mate Striker Brandon Caserta, committed suicide (Kime, 2020). Investigations found that vulgarity, mistreatment and harsh leadership, contributed to the decision Caserta made to take his own life. The Brandon Act would give servicement a safe word to say that would immediately trigger an advancement to see a mental health professional outside of their chain of command (Kime, 2020). The bill, H.R. 7368 is similar to restricted reporting that is already carried out by the military. The bill was designed to ensure that service members can get the mental health help and assistance they need (Kime, 2020).
Military Times.com Patricia Kime, June 2020.
Homelessness for victims of domestic violence, who have children, on the rise amidst the coronavirus pandemic
By Dr. Amber D. Gray
June 2020
According to the California Health Report, organizations are starting to make a push towards ensuring that there are resources on hand to assist victims of domestic violence, who need housing (Boyd-Barrett, 2020). Due to isolation and quarantining efforts, many victims of domestic violence are finding that they are stuck at home more often with their abuser. With little to no options, victims of violence may find that they must leave their homes, to protect themselves, but more often their children. However, this is causing another problem.
Homelessness. While people are able to get themselves to a safe space, “away from the abuser,” they are now finding, that they have no where to go. They are homeless. During the pandemic, there have been fewer places to call to receive resource services (Boyd-Barrett, 2020). The California Office of Emergency Services is seeking to do something about this dilemma, by making housing a priority. For 2020, California’s Office of Emergency Services, was given a grant for $22 million dollars, to assist with the housing first effort. California Governor Gavin Newsom, also announced that more domestic violence support services will be provided for victims, during the Coronavirus pandemic.
As care providers, we are aware of the rises in child abuse, domestic violence, homelessness, racism and other traumatizing social problems. It is good that many of us are rising to the occasion to help to do something about the growing problems within the nation. Making sure that care providers are trauma informed will assist in helping to meet the demands that the pandemic has brought.
Call the National Domestic Violence Hotline, at 1-800-799-7233 to find out what your organization, or you can do to provide assistance during these times. It will take a collaborative effort to make things fall into place. As care professionals, we will approach these crisis, one day at a time, one step at a time, throughout our lives. Be safe!
Sources:
For survivors of violence and their kids, a push to prioritize housing. (2020, June 25). California Health Report. https://www.calhealthreport.org/2020/06/25/for-survivors-of-violence-and-their-kids-a-push-to-prioritize-housing/
SBIRT TRAINING… YES OR NO?
By Dr. Amber D. Gray
May 2020
Primary care providers, allied health professionals, nurses, and other medical providers are often looking for evidence-based, standardized training, that can assist them with patients with substance use issues. In 1999, along came SBIRT. By 2006, medical facilities were required to have their providers trained in SBIRT. Still, little is known about SBIRT outside of the healthcare arena. SBIRT stands for Screening, brief intervention and referral to treatment. It is a care pathway that assist providers in effectively treating patients with substance use issues. Medical professionals who train on the web-based version of the SBIRT training, rate their self-efficacy and knowledge much higher, than before they took the training. As a care provider, it would behoove most practitioners to take the SBIRT training to be more effective in treating their patient populations. Check out: https://sbirt.clinicalencounters.com/
to find out how you can become SBIRT certified.

